Abstract
Introduction. Generic formulations of imatinib mesylate have been introduced in western Europe and the US since 2017 for the treatment of patients affected by Chronic Myeloid Leukemia (CML). Despite bioequivalence data, no independent study to investigate the safety and efficacy of generic imatinib was performed in this region.
Aim of the study. The primary goal of the Generic IMatinib Switch (GIMS) Study is to evaluate the clinical outcome, expressed as variation in quantitative polymerase-chain-reaction (PCR) values, in patients affected by CML treated at 5 Italian institutions belonging to REL (Lombardy Hematological Network), who switched from brand to generic imatinib as first line of treatment. Adverse events (AEs) reported from patients were also tracked and analyzed.
Patients and Methods. This is an observational, multicenter, retrospective analysis of patients affected by CML in chronic phase with stable disease (defined as at least 18 months of complete cytogenetic remission and 36 months of treatment with brand imatinib) who switched from brand to generic imatinib beginning in January 2017. Four manufacturers of generic imatinib were used: Accord, Reddy, Sandoz, Teva. We analyzed the variation of quantitative PCR values, considering BCR/ABL cDNA copies/≥10000 ABL copies corrected by the International Standard (IS). Three PCR values were considered in a period of 12 months before the switch and two to three values in the 12 months following the switch. We evaluated and compared the median PCR values before and after the switch as well as AEs reported with brand and generic formulations. Wilcoxon non parametric test for individual paired data was used to compare the median number of pre switch copies with the number of post switch copies. McNemar non parametric test for paired propotions was used to compare the percentages of patients with AEs. A 5% significance level was considered for two sided test.
Results. PCR determinations from 109 patients were available for the analysis. Median duration of imatinib treatment was 9.1 years (range 4.5-18.3 years). The mean age at the time of the switch was 57 years (range 18-85 years); 46 patients were female (42%), while 63 where male (58%). Of these, 94 patients (86.2%) had all PCR values required, 15 (13.8%) had only two out of three post-switch values. The median value of the three PCR performed before the switch was 1.20x10-4 (range 0 - 236x10-4 ; mean 8.70x 10-4 , SD= ± 26.0x10-4;), while the median value after the switch was 0.51x10-4 (range 0 - 94 x10-4 ; mean 4.08x 10-4, SD= ± 12.14x10-4). Median PCR value after switch was reduced by 0.69 compared to values observed before the switch. A statistically significant difference was found between these values (p<0.0001) in favor of generic imatinib.
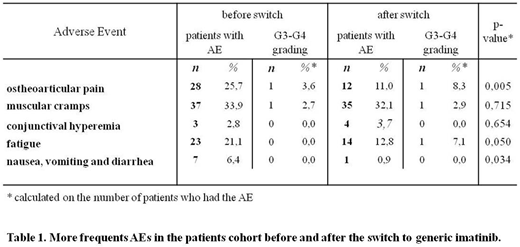
The comparison between pre and post-switch AEs showed a statistically significant difference in favor of generic imatinib for most of them, with the exception of muscular cramps and conjunctival hyperemia. The most frequent AEs are reported in table 1. No patient switched to generic imatinib had to revert to brand imatinib (0%; 95% C.I: 0-2.8%).
Patients receiving generic imatinib in formulations smaller than the brand imatinib formulation reported an easier swallowing of the pills.
Conclusions. Our preliminary data obtained in this cohort of CML patients suggest that generic imatinib does not have deleterious effects on CML control and presents an acceptable safety profile, similar or better than brand imatinib. The statistically significant reduction in PCR values after the switch to generic imatinib must be considered with caution and further data are required to investigate this aspect. These data will be useful to clarify doubts and fears among CML patients about generic imatinib safety and effectiveness.
Gambacorti-Passerini:BMS: Consultancy; Pfizer: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal